Veteran Substance Abuse Statistics: Prevalence, Trends, and Challenges


In This Article
Veterans returning to civilian life can face numerous challenges, and substance abuse is one of the most pressing. From high rates of alcohol misuse to increasing prescription opioid concerns, the data on veterans’ substance use reveals both the scope of the problem and the potential for recovery.
Over the last decade, researchers and public health officials have tracked shifting patterns in veteran substance abuse, highlighting factors such as combat exposure, PTSD, age, and gender.
Understanding these trends is essential for improving prevention, treatment outreach, and long-term support programs aimed at helping veterans lead healthier, more stable lives.
Key Statistics at a Glance:
- Roughly 1 in 10 veterans receiving first-time VA health care services is diagnosed with a substance use disorder.
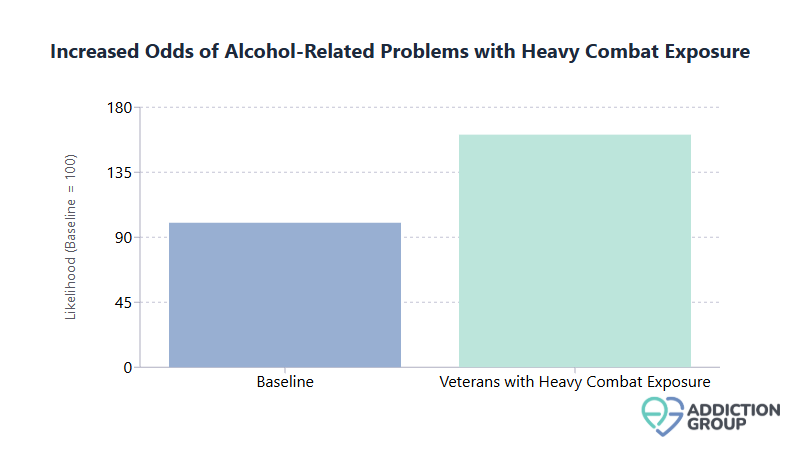
- Veterans with heavy combat exposure face 61% higher odds of developing alcohol-related problems.
- 70% of homeless veterans struggle with a substance use disorder.
- Only about 28 to 30% of veterans with a substance use disorder receive treatment in a given year.
Why This Data Matters
Veterans are a unique demographic with service-related stressors, including combat trauma, multiple deployments, and reintegration difficulties that can elevate substance misuse risks. Tracking the prevalence, types of substances used, and treatment outcomes allows health professionals and policymakers to refine interventions that effectively reduce harm and support long-term recovery.
Service Era Differences
Service era is a strong predictor of substance use risk among veterans. More recent service eras, especially post-9/11, show higher rates of substance misuse compared to earlier cohorts.
- Newer Veterans: Among those who served after September 2001, approximately 12 to 13% report a substance use disorder, nearly double the rate seen in older groups like Vietnam-era veterans.
- Older Eras: Vietnam-era rates can be as low as 4 to 5%, although some older veterans may have experienced more severe substance problems in earlier decades.
These differences often reflect distinct combat environments, multiple deployments, and differences in age. Newer veterans tend to be younger overall, a demographic that consistently shows higher substance use rates than older groups.
Sponsored
Online Therapy Can Help
Over 3 million people use BetterHelp. Their services are:
- Professional and effective
- Affordable and convenient
- Personalized and discreet
- Easy to start
Answer a few questions to get started

Combat Exposure as a Risk Factor
Exposure to intense or traumatic combat scenarios is closely tied to substance misuse, especially heavy drinking. Veterans who have witnessed extreme violence or have had to kill in combat settings frequently report using substances to cope with psychological distress.
- Binge Drinking: Up to 54 to 55% of veterans with significant combat exposure report binge drinking, compared to lower percentages among non-combat personnel.
- Alcohol Problems: Combat veterans have a 61% higher likelihood of developing alcohol-related issues if they directly experience traumatic or morally injurious events.
- Post-Deployment Challenges: About 1 in 10 Iraq and Afghanistan veterans seen in VA healthcare settings have a substance use problem, indicating a direct link to the stressors of deployment.
Sponsored
Get Professional Help
BetterHelp can connect you to an addiction and mental health counselor.
Answer a few questions to get started

PTSD and Substance Abuse
Post-Traumatic Stress Disorder (PTSD) frequently co-occurs with substance misuse in the veteran population, creating a cycle that can be difficult to break without integrated treatment.
- Dual Diagnosis: More than 2 in 10 veterans with PTSD also meet the criteria for a substance use disorder.
- Clinical Overlap: Among veterans seeking help for substance abuse, nearly 30% also have PTSD.
- Elevated Risk: A veteran with a diagnosed substance use disorder is about 3 to 4 times more likely to develop PTSD or depression compared to one without SUD.
Because PTSD symptoms often drive individuals toward self-medication with alcohol or drugs, simultaneous treatment of both conditions is considered best practice.
Treatment Program Outcomes
Veterans have access to evidence-based substance abuse treatment through the Department of Veterans Affairs and community providers. Completion of formal programs is strongly associated with sustained recovery and reduced relapse rates.
- Residential Rehab: Long-term follow-ups show that roughly 30% of veterans who complete a VA residential treatment program remain abstinent over five years, versus near-universal relapse among those who drop out.
- Medication-Assisted Treatment (MAT): Combining medication (like buprenorphine or methadone) with counseling reduces mortality risk in veterans with opioid use disorder by up to 38%.
- Integrated Care Success: Veterans with both PTSD and SUD can achieve recovery outcomes comparable to those with SUD alone when treatment addresses both conditions together.
While relapse is common, particularly in the first year, veterans who remain engaged in aftercare show promising rates of long-term improvement.
Sponsored
Phone, Video, or Live-Chat Support
BetterHelp provides therapy in a way that works for YOU. Fill out the questionnaire, get matched, begin therapy.
Answer a few questions to get started

VA Utilization and Gaps
The VA is a leading provider of addiction services for veterans, yet a significant portion of those in need are not consistently accessing or remaining in specialty care.
- Diagnosis in VA Settings: Approximately 11% of veterans presenting for the first time in VA healthcare have a substance use disorder.
- Numbers in Need: Each year, over 600,000 veterans within the VA system carry an SUD diagnosis.
- Under-Enrollment in Treatment: Only about 30% of veterans identified with SUD through VA screenings actually receive specialized addiction treatment, pointing to gaps in referral and engagement.
Substance Preferences and Trends
Alcohol remains the most prevalent substance of misuse among veterans, but other patterns, especially opioid abuse, have grown in recent years.
- Alcohol Dominance: More than 80% of veterans with a diagnosed SUD cite alcohol as their primary substance. Binge drinking rates in military-affiliated populations exceed many civilian benchmarks.
- Illicit Drugs: Marijuana is the most commonly used illicit drug (over 10% report past-year use). Cocaine and heroin misuse account for a smaller share but often represent more severe addiction cases.
- Prescription Opioids: As many as 41,000 veterans each year struggle with prescription opioid addiction, reflecting an elevated risk from pain treatment. Overdose fatalities related to opioids increased among veterans throughout the early to mid-2010s.
Age Breakdown
Substance use problems are not evenly distributed across age groups. Younger veterans typically exhibit higher rates of misuse, with risks gradually declining as veterans grow older.
- Young Veterans (18 to 25): Nearly 50% of this age cohort reports either a substance use disorder or a related mental health diagnosis, making them the highest-risk group.
- Older Veterans (50+): While SUD rates are relatively low among older veterans, some deal with long-term health complications or chronic conditions from earlier addiction.
Addressing addiction in the critical early years after discharge from service can reduce the long-range health and social impacts of substance misuse.
Gender Differences
Men outnumber women in the overall veteran population, and they also show higher rates of substance misuse. However, drug and alcohol problems are an increasing concern among female veterans as their representation in the military expands.
- Prevalence: Male veterans have approximately double the substance use disorder rate of female veterans.
- Specific Patterns: Alcohol is the most common issue for both men and women, but female veterans may be somewhat more prone to prescription drug misuse, often linked to medical treatment.
- Comorbid PTSD: Women with military sexual trauma or combat-related PTSD frequently report co-occurring SUD, illustrating a need for gender-specific support services.
Homelessness and Substance Use
Substance abuse significantly contributes to homelessness among veterans, forming a deeply interconnected cycle.
- High Correlation: An estimated 70% of homeless veterans have a substance use disorder.
- Bidirectional Risk: Homelessness exacerbates addiction by increasing stress and limiting treatment access, while ongoing substance misuse raises the likelihood of becoming homeless.
- Shelter Admissions: About 1 in 5 veterans in SUD treatment lacks stable housing at the time of admission, underscoring the importance of coordinated housing and recovery services.
Employment and Financial Stability
Trouble holding a steady job is both a cause and a consequence of substance misuse for many veterans.
- Unemployment Link: Unemployed veterans are about twice as likely to have a substance use disorder compared to those who are employed.
- Workforce Reentry: Among veterans entering substance abuse programs, only 28% report any paid work in the month before treatment. This number may rise to roughly 35% after discharge but remains an ongoing challenge.
- Co-Occurring Issues: Chronic pain, PTSD, and depression often compound job instability, making targeted vocational rehabilitation critical.
Family and Relationship Strains
Addiction can disrupt veterans’ relationships, parenting responsibilities, and marital stability, with ripple effects that last for years.
- Marital Instability: Divorce rates among veteran families can be several times higher than in the general population, partly driven by substance misuse and underlying mental health conditions.
- Parenting Concerns: Child protective services may become involved when veterans’ addiction impairs their ability to provide a safe environment.
- Protective Factors: Healthy family support can serve as a buffer against substance misuse. Married or partnered veterans typically have lower rates of SUD than single or divorced individuals, though this advantage reverses once chronic misuse takes hold.
Access to Support Services
Despite the availability of VA and community-based programs, most veterans with substance use disorders do not receive formal treatment in a given year.
- Under-Treatment: Around 70% of veterans with an active SUD go without specialized care each year.
- Perceived Need: A striking 94% of those who skip treatment report believing they do not need professional help, highlighting low problem recognition.
- Stigma Barriers: Concerns about career impact, cultural attitudes toward seeking help, and logistical barriers (such as clinic distance or scheduling conflicts) keep many from utilizing VA and other services.
Long-Term Recovery and Success Rates
Recovery from substance abuse is achievable but often requires sustained treatment engagement and continued support.
- Treatment Completion: About 30% of veterans who finish a residential SUD program remain abstinent over five years compared to near-zero among those who drop out early.
- Relapse Patterns: Relapses frequently occur within the first year. Nonetheless, long-term tracking shows that those who maintain recovery for 12+ months have a significantly higher chance of remaining sober.
- Integrated Supports: Factors like stable housing, employment assistance, peer support, and family involvement greatly enhance the likelihood of long-term success.
Geographic Distribution Factors
Rates of substance misuse and the types of substances used can vary by region, as can accessibility of treatment.
- Regional Opioid Prescribing: VA facilities in the western and southern United States historically prescribed higher volumes of opioids, correlating with higher incidences of opioid use disorder.
- Rural vs. Urban: Rural veterans often face longer travel times for care and may receive more opioid prescriptions for chronic pain, while urban veterans are more likely to encounter illicit substances like cocaine or heroin.
- Availability of Services: Large urban areas typically have major VA medical centers, whereas rural veterans rely heavily on smaller clinics or telehealth options.
Long-Term Outcomes
For veterans who struggle with addiction, the long-term trajectory varies widely, spanning chronic health problems to successful recovery stories.
- Health Implications: Early and prolonged abuse can lead to conditions like liver cirrhosis, cardiovascular disease, or hepatitis C, persisting well after someone stops using.
- Mortality Risk: Substance abuse elevates rates of accidental death, suicide, and overdose. Some estimates attribute up to 30% of veteran suicides to drug or alcohol involvement.
- Positive Recovery Paths: Veterans who remain abstinent for multiple years can see improvements in overall health, re-employment, and stable family relationships. Peer mentorship and continued counseling are central to sustaining these gains.
| Category | Notable Figures | Significance |
| Alcohol Misuse | 80%+ of veteran SUD cases | Highest cause of substance-related health costs |
| Homelessness | 70% have SUD | Highlights need for integrated housing programs |
| Treatment Gap | ~70% go untreated | Stigma and low perceived need limit care |
| Residential Rehab | 30% remain abstinent long-term | Shows efficacy of full treatment completion |
(Table: Key metrics illustrating scope, impact, and outcomes of veteran substance abuse.)
Over the years, researchers, veteran advocacy groups, and the VA have pushed to refine interventions based on these statistics. The figures serve as a reminder that substance abuse among veterans is not an isolated phenomenon but is inextricably linked to issues like mental health, economic stability, and familial support.
Ultimately, continuing to track and analyze these statistics is vital for optimizing care models. Enhanced data collection and evidence-based treatments not only empower veterans to regain control over their lives but also ease the public health and economic burdens felt by local communities and the nation at large.
Looking ahead, stakeholders will need to bolster outreach efforts, dismantle stigma within military and veteran cultures, and coordinate services that address the multifaceted needs of those in crisis. By applying the lessons gleaned from these statistics, communities can work together to transform the challenges of addiction into stories of resilience and renewal.
What's Next?
Sponsored
Get matched with an affordable mental health counselor
Find a TherapistAnswer a few questions to get started

Related Articles

The Pandemic's Toll: Substance Abuse and Addiction Trends During COVID-19

Benzodiazepines Addiction: Statistics and Effects

Substance Abuse and Domestic Violence: National Statistics

Updated Overdose Statistics 2025: Trends in Drug-Related Deaths

Addiction Treatment: Statistics on Efficacy

Addiction Statistics in Australia
- Centers for Disease Control and Prevention (CDC) – https://www.cdc.gov/data-statistics
- National Institute on Drug Abuse (NIDA) – https://nida.nih.gov/research-topics/substance-use-military-life
- National Survey on Drug Use and Health (NSDUH), SAMHSA – https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report
- PubMed Database – https://pubmed.ncbi.nlm.nih.gov
- U.S. Department of Health & Human Services (HHS) – https://www.hhs.gov/opioids/
- U.S. Department of Veterans Affairs (VA) National Center for PTSD – https://www.ptsd.va.gov

