Mental Health and Substance Abuse: National Statistics


In This Article
Mental health disorders and substance abuse are critical public health challenges that often intertwine to create complex, co-occurring conditions.
Although awareness and treatment strategies have improved in recent years, millions of Americans still struggle to access the care they need and sustain long-term recovery.
In the following overview, we will examine current data on mental health and substance abuse rates, the populations most affected, the economic burden these issues impose, and the array of interventions that offer hope for sustainable recovery.
By highlighting key statistics and exploring major influencing factors, we can better understand the scale of these conditions and the multifaceted steps required to address them.
Noteworthy Statistics at a Glance
- Over 8% of U.S. adults report having both a mental health condition and a substance use disorder in a given year.
- Fewer than 1 in 6 individuals with co-occurring disorders receive treatment for both conditions.
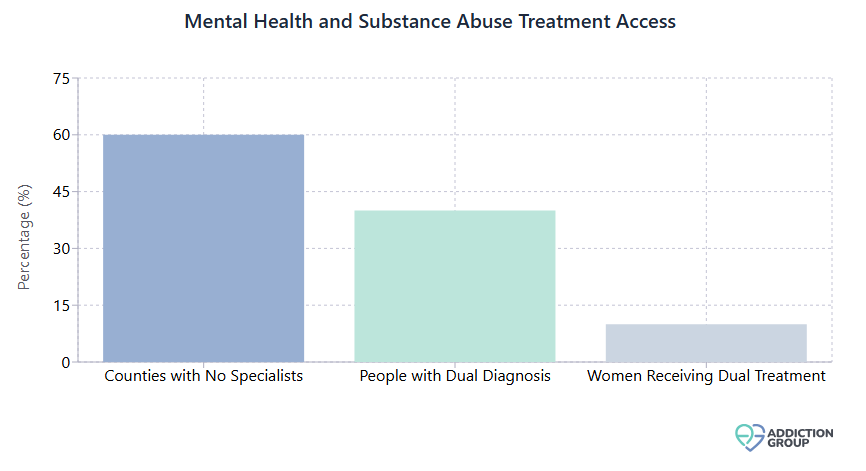
- Approximately 60% of U.S. counties have no practicing addiction medicine specialists.
- Women with co-occurring disorders are particularly underserved, with over 90% not receiving dual treatment services each year.
The Scope of Co-Occurring Disorders
Co-occurring disorders, also called dual diagnoses, refer to the presence of a mental health condition and a substance use disorder at the same time. This overlap is increasingly recognized as one of the most pressing public health challenges in the country. When these disorders intersect, each can exacerbate the other, making effective treatment and sustained recovery much more difficult.
Prevalence and Rising Awareness
- According to national surveys, as many as 1 in 12 adults may experience co-occurring mental illness and substance abuse in a given year.
- Over 40% of individuals diagnosed with a substance use disorder also have at least one mental health condition.
- Reported rates of dual diagnosis have increased in the last decade, a trend attributed partly to better screening and partly to rising substance use among younger populations.
Collectively, these findings underscore the importance of integrated approaches in mental health and addiction services, as treating only one condition often leaves the other unaddressed.
Demographic Insights
- Young Adults (18 to 25): This group exhibits some of the highest rates of co-occurring disorders. Substance use among emerging adults has jumped by more than 30% over the past decade, in parallel with rising mood and anxiety disorders.
- Middle-Aged Adults (26 to 49): Stressors such as employment insecurity and financial pressures contribute to higher rates of alcohol, opioid, and prescription medication misuse, often coinciding with depression or anxiety.
- Older Adults (50+): Historically underdiagnosed, this population faces unique challenges, including late-onset alcoholism tied to retirement or bereavement and potential misuse of prescription sedatives.
Sponsored
Online Therapy Can Help
Over 3 million people use BetterHelp. Their services are:
- Professional and effective
- Affordable and convenient
- Personalized and discreet
- Easy to start
Answer a few questions to get started

Key Drivers Behind Mental Health and Substance Abuse Patterns
Early Onset and Developmental Factors
One crucial factor shaping these trends is the age of onset. Many psychiatric conditions (including anxiety, mood disorders, and attention-deficit/hyperactivity disorder) surface during adolescence or early adulthood.
Because this stage is also a high-risk period for experimenting with drugs or alcohol, individuals with early mental health symptoms frequently turn to substances to self-medicate.
- Adolescents with untreated mental illnesses have up to a 50% chance of developing a substance use disorder by adulthood.
- Conversely, frequent substance use in the teenage years can precipitate latent psychiatric issues - heavy cannabis use, for example, is linked with higher risks of psychosis in genetically predisposed teens.
When either condition develops at a young age, it amplifies the risk for the other, illustrating why early intervention is a leading strategy for reducing lifelong complications.
Gender Disparities
Men and women experience mental health and addiction in distinct ways:
- Men: Generally have higher rates of illicit drug use and are more prone to externalizing disorders (e.g., antisocial behavior). They are also more likely to be incarcerated or face legal issues related to substance misuse.
- Women: Show higher rates of depression and anxiety and frequently misuse prescription sedatives or pain relievers. Over 90% of women with co-occurring disorders reportedly do not receive comprehensive dual treatment, often due to childcare barriers or stigma.
Tailoring interventions to account for these differing patterns can significantly improve overall treatment adherence and success.
Socioeconomic Influences
Socioeconomic status (SES) strongly affects both risk and treatment outcomes:
- Individuals living below the poverty line have notably higher rates of serious mental illness and drug use, often tied to chronic stress, trauma, and limited healthcare access.
- Homeless populations show among the highest rates of co-occurring disorders, frequently cycling between emergency departments, shelters, and jails without long-term stability.
- Unemployment or low-wage jobs exacerbate mental health symptoms and heighten the likelihood of self-medication with substances, perpetuating a cycle of financial and social instability.
Thus, strategies that incorporate housing support, employment assistance, and integrated case management are pivotal in breaking the link between economic hardship and dual disorders.
Sponsored
Get Professional Help
BetterHelp can connect you to an addiction and mental health counselor.
Answer a few questions to get started

Highlighting Financial and Societal Costs
High Healthcare Utilization
- The medical costs for individuals struggling with both addiction and mental illness can be nearly double those of treating either condition alone.
- Repeated use of inpatient and emergency services inflates healthcare spending. National estimates suggest substance-related ER and hospitalization costs exceed $13 billion per year, with co-occurring disorders adding to that figure.
Broader Economic Impact
- Lost productivity: Many with dual diagnoses find it challenging to maintain stable employment, leading to reduced economic output.
- Criminal justice expenses: Individuals with co-occurring disorders have a higher likelihood of arrest, especially if their conditions go untreated. This leads to increased corrections spending.
- Strain on families: Households often shoulder the expense of private rehab, repeated hospital visits, or long-term therapy, sometimes plunging into debt or forgoing needed services because of cost barriers.
Quality of Life Consequences
Beyond direct monetary costs, unaddressed mental health and substance issues can result in elevated rates of homelessness, family disruption, and overall decreased life satisfaction.
By investing in effective integrated interventions, communities can decrease the long-term financial and social burdens associated with repeated crises and relapses.
Approaches to Treatment and Long-Term Recovery
Modern best practices emphasize integrated treatment, where mental health care (e.g., therapy, psychiatric medication) and addiction services (e.g., detox, medication-assisted treatment, relapse prevention) are offered in tandem.
1. Inpatient (Residential) Rehab
- Benefits: 24/7 structured environment, safe detox from substances, and immediate stabilization for acute psychiatric symptoms.
- Challenges: High cost, need for insurance coverage or self-pay, and risk of relapse post-discharge if aftercare is weak.
2. Outpatient Programs
- Standard Outpatient: Weekly or biweekly therapy and medication management. Ideal for less severe cases or as step-down care from inpatient.
- Intensive Outpatient (IOP)/Partial Hospitalization (PHP): Multiple sessions per week, combining individual and group therapy, relapse prevention training, and psychiatric consultation.
Outpatient models are often more sustainable, allowing patients to practice sobriety skills in daily life. However, they rely heavily on patient motivation, stable housing, and robust support systems.
3. Pharmacological Interventions
Medication can be essential for certain co-occurring diagnoses:
| Medication Type | Primary Use | Key Example |
| Antidepressants | Alleviate depression and anxiety symptoms | SSRIs (e.g., sertraline) |
| Mood Stabilizers | Control bipolar mood swings and reduce manic episodes | Lithium or valproic acid |
| Antipsychotics | Manage symptoms of schizophrenia or severe bipolar mania | Long-acting injectable risperidone |
| Medication-Assisted Treatment (MAT) | Reduce cravings/withdrawal in opioid or alcohol use disorders | Buprenorphine, naltrexone, or acamprosate |
- Example Impact: MAT for opioid use disorder has been shown to cut mortality rates by more than half and significantly reduce relapse.
The combination of evidence-based therapy with the appropriate medication regimen yields better outcomes than relying on psychosocial support or medication alone.
Sponsored
Phone, Video, or Live-Chat Support
BetterHelp provides therapy in a way that works for YOU. Fill out the questionnaire, get matched, begin therapy.
Answer a few questions to get started

Barriers to Access and Potential Solutions
Despite emerging best practices, access to dual-diagnosis treatment remains uneven nationwide. Key barriers include:
- Insurance Limitations: Coverage often falls short for comprehensive, long-term care, particularly integrated programs that blend mental health and addiction services.
- Provider Shortages: An estimated 60% of U.S. counties lack a trained addiction specialist or sufficient psychiatric services, creating long waitlists or forcing patients to travel hours for care.
- Stigma: Fear of judgment or legal consequences keeps some individuals from disclosing substance use or psychiatric symptoms, leading to delayed treatment until crises occur.
- Fragmented Systems: Many clinics address mental health and substance abuse separately, leaving patients to navigate disjointed referrals and potentially give up.
Strategies to Improve Accessibility
- Telehealth Expansion: Video-based counseling and digital medication management can reach rural and underserved populations, cutting down on travel time.
- Integrated Clinics: Co-locating mental health and addiction professionals provide one-stop care, reducing dropout rates.
- Peer Recovery Services: Community-based support groups and peer mentors can boost engagement by offering role models and practical guidance.
- Workforce Development: Training more dual-credentialed providers, especially in rural regions, can bolster local care capacity and reduce patient travel burdens.
Family and Peer Support as Key Recovery Catalysts
Social support is a powerful predictor of successful outcomes. Many who struggle with co-occurring disorders benefit enormously from a caring network:
- Family Involvement: Families participating in psychoeducation and counseling programs can help monitor medication schedules, discourage substance use triggers at home, and offer vital emotional backing.
- Peer Groups: Support communities, such as 12-step fellowships or specialized “dual recovery” meetings, provide camaraderie, shared experiences, and relapse-prevention tools.
- Community Resources: Housing assistance, vocational training, and case management all expand “recovery capital,” helping individuals rebuild stable lives free from constant crisis.
Studies consistently show that individuals with strong social support have fewer relapses, greater medication adherence, and improved overall mental health.
Tracking Long-Term Outcomes
Relapse and Chronic Management
Relapse rates for substance use alone run 40 to 60% in the first year post-treatment, mirroring other chronic illnesses like diabetes. Co-occurring mental illness often increases the risk of early relapse. Yet with sustained, continuous care, and particularly with family and peer support, long-term recovery rates improve significantly.
Quality of Life Metrics
- Stable Housing: Reductions in homelessness and increased ability to live independently.
- Employment/Education: Return to work or school fosters a sense of purpose and financial stability.
- Physical Health: Co-occurring disorder treatment often alleviates other health complications, lowering emergency medical visits and reducing the risk of overdose.
Data on 5-Year Success
While exact numbers vary, many clinicians report that if a person with a dual diagnosis can maintain roughly 5 years of successful management (with or without occasional lapses), the odds of ongoing stability grow substantially.
Similarly, early detection and continuous engagement can transform what might otherwise become a lifelong cycle of relapse and crisis. When all is said and done, co-occurring mental health and substance abuse disorders do not have to be lifelong sentences.
With timely, evidence-based interventions, plus a supportive network, countless individuals achieve enduring stability, meaningful relationships, and renewed productivity.
In the broader context of public health, these statistics underscore the importance of reducing stigma, addressing systemic treatment gaps, and investing in comprehensive, integrated services that treat the whole person.Recovery, of course, is a deeply individual journey. Some will see rapid improvements with structured treatment, while others may need multiple attempts or ongoing support. Multi-pronged approaches can and do work, offering hope to millions affected by co-occurring conditions across the United States.
What's Next?
Sponsored
Get matched with an affordable mental health counselor
Find a TherapistAnswer a few questions to get started

Related Articles

Addiction Statistics in Australia

Statistics on the Impact of Substance Abuse on Crime Rates

The Relationship Between Substance Abuse and Academic Performance

Gender Differences in Substance Abuse and Addiction: Statistics

Updated Overdose Statistics 2025: Trends in Drug-Related Deaths

What Is the Impact of Parental Substance Abuse on Children?
- “Co-Occurring Disorders and Other Health Conditions.” SAMHSA.
- “Common Comorbidities with Substance Use Disorders Research Report Part 1: The Connection Between Substance Use Disorders and Mental Illness.” NIDA.
- “HHS, SAMHSA Release 2022 National Survey on Drug Use and Health Data.” SAMHSA, 2023.
- “Comorbidity: Substance Use and Other Mental Disorders.” NIDA.
- “SAMHSA Announces National Survey on Drug Use and Health (NSDUH) Results Detailing Mental Illness and Substance Use Levels in 2021.” HHS.gov, 2023.
- “Co-curring psychiatric and substance use disorders.” DMH.

